An integrative approach to cancer…
- Combines conventional, self, and complementary care into an integrated whole.
- Improves treatment outcomes, makes your body less supportive of cancer, manages side effects, reduces the risk of recurrence, and, whenever possible, prevents or decreases the risk of adverse long-term and late effects of cancer and its treatment.
- Puts you, the person with cancer, at the center as an active participant in your cancer care.
- Is grounded in evidence or best practices in patient care.
- Is anchored in health and healing, focusing where possible on enhancing your innate capacity to heal physically, mentally, emotionally, and spiritually.
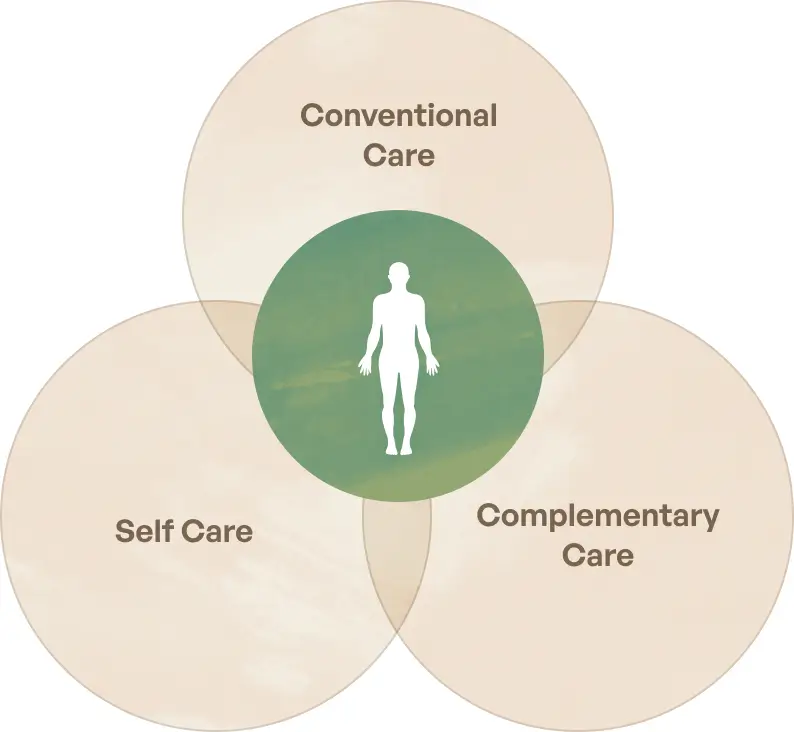
Conventional care is the care you’ll receive from conventionally trained physicians (also called allopathic or Western medicine physicians) and most hospitals. Conventional approaches include surgery, chemotherapy, radiotherapy, and other treatments.
Self care, also called lifestyle medicine, includes your practices and behaviors regarding diet, exercise, relaxation, and more.
Complementary care adds to or “complements” conventional care and includes supplements and other natural products, mind-body approaches such as yoga or psychosocial therapy, energy therapies, special diets, and more.
Integrative cancer care promotes healing
An integrative cancer care approach can reduce your side effects, increase your resilience, and/or prevent or delay recurrence, and potentially extend your life. Conventional, complementary, and self care may affect your cancer experience or impact cancer directly in several ways.
Improves treatment outcomes
Improving treatment outcomes involves promoting survival, reducing metastases, slowing or reversing tumor growth, or reducing tumor markers. Conventional treatments offer the best option for cure or remission for many types of cancer. Wise use of complementary and self care may enhance the effectiveness of conventional treatments. They may also provide support when conventional treatments are not a good choice—such as when potential harms outweigh the expected benefits—or are not available.
Optimizes body terrain
All three approaches—conventional care, self care, and complementary care—can contribute to creating an environment within your body that is less supportive of cancer development, growth, or spread. Integrative, naturopathic, and functional medicine physicians and professionals tend to emphasize and help you balance your body terrain. Conventional medicine places less emphasis here. You can be an active player in this area, as self care is central to optimizing your body terrain.
Promotes wellness
Side effects commonly experienced with conventional treatment can often be reduced or even avoided with complementary and self-care approaches. Complementary therapies are also less likely than conventional therapies to cause side effects when used for treating anxiety, vomiting, sleep disruption, and other common situations. Complementary and self-care approaches can enhance your overall quality of life and general well-being.
Reduces cancer risk
Conventional, complementary and self care can work together to reduce your risk of cancer, recurrence, or a secondary cancer. Complementary and integrative cancer care tend to place more ongoing emphasis and effort here than conventional care.
Supports whole-person healing
Complementary and self care can support your mental, emotional, and spiritual levels of healing, typically more so than conventional care.
Offers grounded hope
If conventional options are limited for your type or stage of cancer, complementary and self care can offer additional avenues for healing and potentially extend and expand your life.
Commentary
CancerChoices Senior Clinical Consultant Laura Pole, RN, MSN, OCNS, wrote a blog post explaining the difference between integrative cancer care and alternative care.
“Many use the terms ‘complementary’ and ‘alternative’ interchangeably, but they indicate different uses of therapies. When a therapy or self-care practice is used in an intentional way along with conventional treatment, it is considered complementary. A therapy or practice used instead of conventional treatment is considered alternative. So it’s not the therapy or practice itself, but how it’s used that makes the difference.”
Read the blog post: Integrative Oncology Is Not Alternative Medicine ›
CancerChoices advisor Keith Block, MD, discusses how the avoidance of conventional therapies in cancer care reduces survival. He also explains the key characteristics of integrative cancer care, distinguishing it from alternative medicine and CAM (complementary and alternative medicine).
Play videoWords of guidance
Read words of inspiration and guidance from Michael Lerner, CancerChoices co-founder and author of Choices in Healing.
Learn more
Helpful links

Semeniuk G, Bahadini B et al. Integrative oncology and the clinical care network: challenges and opportunities. Journal of Clinical Medicine. 2023 Jun 9;12(12):3946.
Videos
Whole Person Cancer Care
Integrative physician and CancerChoices advisor Wayne Jonas, MD, speaks about whole-person cancer care.
Play videoGet Well and Stay Well with Dr. Wayne Jonas & Laura Pole, RN, MSN, Chef
CancerChoices Senior Clinical Consultant Laura Pole talks with Dr. Wayne Jonas about integrative approaches in cancer care.
Play videoLindsay McDonell
Your Dance with Cancer: A Conversation with a Metastatic Breast Cancer Thriver
Play videoSuz Mondello
Creating My Integrative Approach to Cancer Care
Play video