Integrative oncology overview for professionals
What is integrative oncology?
Defining integrative oncology
Integrative oncology has various definitions that have common threads. Integrative cancer care:
- Is patient-centered
- Is informed by evidence
- Includes conventionalthe cancer care offered by conventionally trained physicians and most hospitals; examples are chemotherapy, surgery, and radiotherapy (standard) cancer care
- Includes lifestyle practices (self carelifestyle actions and behaviors that may impact cancer outcomes; examples include eating health-promoting foods, limiting alcohol, increasing physical activity, and managing stress)
- Includes complementaryin cancer care, complementary care involves the use of therapies intended to enhance or add to standard conventional treatments; examples include supplements, mind-body approaches such as yoga or psychosocialtherapy, and acupuncture therapies and practices
- Supports quality of life
- Improves wellness and resilience
- Improves clinical outcomes
Two integrative oncology organizations provide these definitions:
The Society for Integrative Oncology defines integrative oncology as “a patient-centered, evidence-informed field of cancer care that utilizes mind and body practices, natural products, and/or lifestyle modifications from different traditions alongside conventional cancer treatments. Integrative oncology aims to optimize health, quality of life, and clinical outcomes across the cancer care continuum and to empower people to prevent cancer and become active participants before, during, and beyond cancer treatment.”1Witt CM, Balneaves LG et al. A comprehensive definition for integrative oncology. Journal of the National Cancer Institute Monographs. 2017 Nov 1;2017(52).
The Oncio app’s definition: “Integrative oncology (IO) is a patient-centred, evidence-informed field of cancer care that utilises nutrition, lifestyle, psycho-emotional wellbeing and complementary medicine interventions alongside conventional cancer treatments to support better quality of life, improve resilience, minimise the side effects of treatment and improve outcomes.”2Oncio. An integrative approach. Viewed October 3, 2023.
Professional oncology organizations such as the Oncology Nursing Society (ONS), the Academy of Oncology Nurse & Patient Navigators (AONN), and the American Society of Clinical Oncology (ASCO), as well as major cancer centers › are taking this approach seriously. Evidence-based professional organizations such as the Society for Integrative Oncology (SIO) now exist to advance the field of integrative cancer care.
You can put these definitions in patient-friendly language: Integrative oncology has its place beginning with cancer prevention and continuing through treatment, survivorship, and up through the last moments of a person’s life. Blending the best of conventional treatment with self-care practices and complementary therapies creates a greater chance for optimizing health and quality of life as well as treatment outcomes.
Clarify that integrative whole-person cancer care combines carefully chosen conventional/standard treatment with complementary therapies and self-care practices. Simply adding complementary therapies or lifestyle practices without any thought to safety and effectiveness or coordination of care is not an integrative approach.
You can go on further to explain to your interested patients that complementary therapies are those that complement and go hand-in-hand with conventional treatments. Examples include medicinal herbs, mind-body approaches such as relaxation techniques, and body-based methods such as massage. Let patients know that self-care practices support health and well-being, such as eating well, moving more, and managing stress.
For your deeper understanding, we unpack the common elements in the definitions a bit.
Patient-centered: Integrative oncology is focused on the patient. Knowing the person who has the disease is as important as knowing about the disease and its treatment. What really makes integrative oncology work is that it empowers patients to be active participants rather than passive recipients of care.
Example: Your patient is having a challenging time with anxiety. In talking with him, you learn that he really enjoys being outside in nature. You share that modest evidence shows that getting out in nature and even just listening to nature sounds can help manage anxiety. You encourage him to get out in nature when feeling anxious and provide him with an audio recording of nature sounds to listen to when he can’t get out. You schedule to follow up with him in two weeks.
Evidence-informed: Integrative practitioners base information, advice, and therapy recommendations on scientific evidence. The level of rigorous evidence needed to support the use of a therapy is proportional to both the likely benefit and the risk of harm from using the therapy. Treatments such as chemotherapy or radiation that may cause substantial side effects or carry other risks require strong scientific evidence of benefit to determine if the benefits outweigh the risks.
On the other hand, therapies that generally promote health without bringing substantial risk may not need the same level of evidence. Thus, the evidence base for many of these therapies and practices does not need to be as robust. However, some complementary therapies may involve risks, including interactions with conventional treatments or with other therapies or medications, risks for people with some medical conditions, and so on. Simply piling complementary therapies onto conventional treatment without looking at possible interactions, side effects, and contraindications is not appropriate. Therefore, an evidence-informed approach to choosing complementary and self care, including considering both benefits and risks, is still important.
Only a fraction of research dollars go toward studying safety and effectiveness of complementary therapies. Because rigorous research is limited, we promote a broader evidence-informed approach that includes more types of evidence, such as use by integrative medical experts. CancerChoices clearly separates and rates these different types of evidence so our readers can assess a therapy according to their own values and priorities.
Even further types of evidence beyond published research and expert recommendations include the clinician’s experience and the patient’s general health, psychosocial and financial situation, previous experiences, and access to services.
Including all these types of evidence, from rigorous research evidence to clinician and patient factors, is an “evidence-informed” approach to cancer care. An evidence-informed approach could identify safe and likely effective therapies in cancer care that do not yet have rigorous research supporting use.
Example: Your patient is asking for help managing fatigue. They’re interested in non-drug approaches, although they’ve never done any mind-body approaches. You see that a few studies suggest qigong is likely to be helpful with quality of life, it may help fatigue, and it’s generally safe. The risks and benefits indicate that qigong could be a good complementary therapy to try alongside chemotherapy. You discuss the benefits and any specific concerns you might have for your patient. Your patient is willing to try it. You refer your patient to online teachers who work with people with cancer and you ask your patient to follow up with you in three weeks.
Integrative oncology treatment approaches: We use the word “Integrative” because this type of care integrates complementary therapies and lifestyle practices with conventional treatment. All three approaches are used within one overall plan that coordinates the effects, doses, timing, and benefits of each approach while minimizing interactions and risks.
Traditional medical systems, such as traditional Chinese medicine or Ayurveda, have a lot to offer people with cancer. More and more, these systems are blended in with conventional treatment, such as using acupuncture for bone-related pain caused by aromatase inhibitors ›.
Integrative cancer care combines conventional treatment, complementary therapies, and self-care practices in a coordinated, purposeful approach to cancer care and wellness.
For help explaining integrative oncology to your patients, see Integrative Cancer Care ›
Integrative oncology is not alternative medicine
A therapy used in an intentional way alongside conventional therapy is considered complementary. A therapy used instead of conventional treatment is considered alternative. So the therapy itself is not complementary or alternative, but how it’s used. For instance, using a diet as a stand-alone treatment for cancer would be considered an alternative use. The same diet, however, might be recommended as an adjunct to cancer treatment and would be complementary.
For information to share with your patients who are considering alternative therapies, see When Conventional Treatments Are Not an Option ›
Why integrative oncology
The number of people diagnosed with and living longer with or beyond cancer is increasing. As a result, more people want to focus on long-term issues relating to quality of life. Many people are looking for a better way—a way that treats them as a whole person. They want to focus not only on cure but also healing. An integrative approach may improve the chances for better treatment outcomes, quality of life, symptom management and risk reduction while focusing on the whole person.3Crudup T, Li L et al. Breast cancer survivorship and level of institutional involvement utilizing integrative oncology. Journal of Oncology. 2021 Dec 18;2021:4746712.
With information and research readily available online, people are doing their own searches and finding that their oncology team may not be focused on all aspects of the care they believe they deserve. When health or life are threatened, many people want to do everything within their means, both conventional and non-conventional, to live and live well.
In too many cases, an oncology care team is often not aware that their patients are using complementary and self care.4The ASCO Post Staff. Use of Integrative Medicine by Patients with Breast Cancer. The ASCO Post. June 7, 2021. Viewed October 4, 2023; Crudup T, Li L et al. Awareness, perceptions, and usage of whole person integrative oncology practices: similarities and differences between breast cancer patients and oncologists. Journal of Clinical Oncology. 2021;39:15. As a result, the different aspects of cancer care are not coordinated and therefore not integrative.
Patients want a better way to live with and beyond cancer. Integrative oncology offers the hope of a better way.
As health professionals, becoming more open-minded and integrative in our approach to cancer care can allow those we serve to feel like they don’t need to be closeted users of complementary therapies and self-care practices.
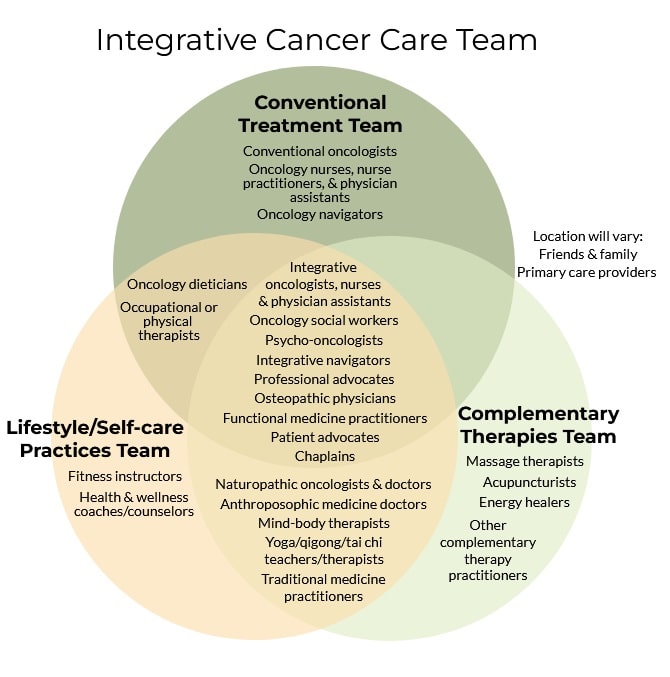
Who provides integrative oncology
Integrative oncology care delivery spans a continuum. On one end is a conventional oncology treatment center that refers people out to and works collaboratively with integrative oncology specialists. On the other end are cancer centers that are staffed with integrative oncologists and practitioners. Somewhere in between are the many cancer centers that offer lifestyle and self-care education and coaching programs specifically for people with cancer.
Some of the many different professionals who provide some facet of integrative care to cancer patients:
- MD, DO, and naturopathic (ND, FABNO) integrative oncologists, integrative medicine physicians
- Advanced practice nurses and physician assistants
- Doctors of Oriental Medicine and other traditional medicine practitioners
- Other practitioners trained in integrative medicine, functional medicine, holistic medicine/nursing, lifestyle medicine
- Complementary medicine practitioners
- Integrative oncology navigators, coaches, advocates, or educators
If you provide conventional treatment exclusively, and your patients want to add evidence-based complementary and self care to the plan, you can serve them by:
- Referring them to trusted integrative oncologists and/or other integrative/holistic physicians/practitioners, complementary therapy practitioners (such as oncology massage therapists) and self-care/lifestyle medicine programs in your community. For more information on who practices integrative oncology and how to find practitioners, see Finding Integrative Oncologists and Other Professionals ›
- Referring them to How to Integrate Your Choices › to learn more about making skillful decisions about cancer treatment, integrative medicine at NCI-designated cancer centers, and more.
Health professional comment
We invite health professionals to contribute expertise or send us questions.
"*" indicates required fields
References
