Why are high blood sugar and insulin resistance important?
High blood sugar and/or insulin resistance can affect cancer risk and outcomes, plus other body terrainthe internal conditions of your body, including nutritional status, fitness, blood sugar balance, hormone balance, inflammation, and more factors connected to cancer.
Direct connections to cancer
Chronically high blood sugar may accelerate cancer progression, invasion, and migration to other areas of the body. High blood sugar may also help cancer cells resist normal cell death and may promote resistance to chemotherapy. It prompts the body to produce substances that promote inflammation and may be linked to development of tumors.1Li W, Zhang X et al. Effects of hyperglycemia on the progression of tumor diseases. Journal of Experimental & Clinical Cancer Research. 2019 Jul 23;38(1):327.
“Insulin increases cell production and reduces cell death”2Underferth D. Sugar, insulin resistance and cancer: What’s the link? MD Anderson Cancer Center. June 21, 2021. Viewed August 12, 2022.—two hallmarks of cancer. Relatively small but chronic rises in blood sugar or insulin may contribute to cancer growth.3Mulholland HG, Murray LJ, Cardwell CR, Cantwell MM. Dietary glycaemic index, glycaemic load and endometrial and ovarian cancer risk: a systematic review and meta-analysis. British Journal of Cancer. 2008 Aug 5;99(3):434-41. Chronic high levels of insulin are linked to diabetes and several types of cancer.4Yin M, Zhou J, Gorak EJ, Quddus F. Metformin is associated with survival benefit in cancer patients with concurrent type 2 diabetes: a systematic review and meta-analysis. Oncologist. 2013 Dec;18(12):1248-1255; Underferth D. Sugar, insulin resistance and cancer: What’s the link? MD Anderson Cancer Center. June 21, 2021. Viewed August 12, 2022.
Managing high blood sugar and insulin resistance is very important for reducing your risk of poor cancer outcomes. A combination of self-care practices including Eating Well and Moving More, medication use as directed by your physician, and use of appropriate complementary therapies, all carefully monitored by your physician, can improve your levels and reduce your risk of poor cancer outcomes. See What approaches can help you manage high blood sugar and insulin resistance? ›
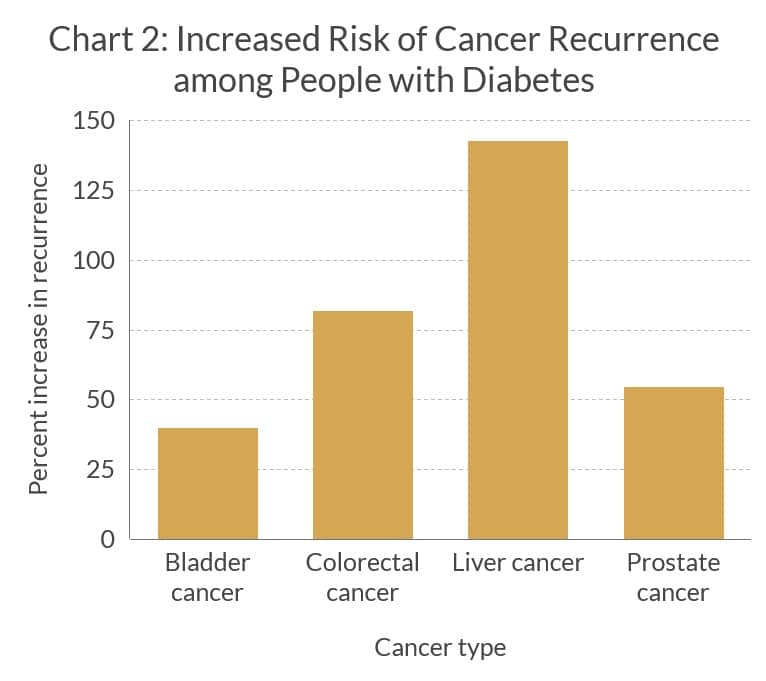
Largely due to increased blood sugar and insulin resistance, people with diabetes are at higher risk of poor cancer outcomes compared with nondiabetic people with cancer, as shown in these charts.
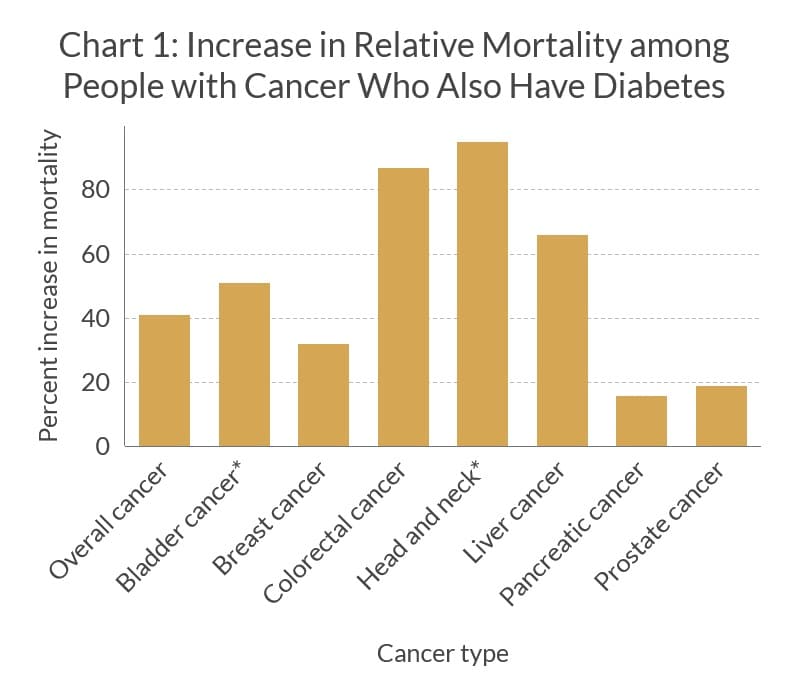
*Cancer-specific survival; all others are overall survival
Note: Studies, detailed below, reported different mortality time points, from one year to more than eight years. Some studies reported mortality among more specific populations, such as people at a specific cancer stage or with a specific subtype of cancer. When more than one study reported differing numbers on mortality, we used the more conservative numbers.
Connections to body terrain factors
Hyperglycemia and insulin resistancea condition in which cells in your muscles, fat, and liver don’t respond well to insulin and can’t efficiently take up glucose from your blood for energy have links to all the other body terrainthe internal conditions of your body, including nutritional status, fitness, blood sugar balance, hormone balance, inflammation and more factors. Sometimes the cause and effect are seen in both directions (bidirectional). Sometimes an imbalance in one terrain factor causes a domino effect, toppling the balance of other terrain factors. Details of these connections follow, but first we want to emphasize the web of connections among factors that aren’t as apparent by looking at factors one at a time.
For instance, hyperglycemia and insulin resistance trigger a cascade of immune events that promote inflammation, which, along with oxidative stressan imbalance between free radicals and antioxidants in your body in which antioxidant levels are lower than normal; this imbalance can cause harmful oxidation reactions in your body chemistry can then damage the inside of blood vessels and lead to coagulation problems such as developing blood clots along the lining of these vessels. While the “fires of inflammation” are burning, other immune functions, such as protection against infection, may be hampered by uncontrolled hyperglycemia and insulin resistance. People with diabetes are at higher risk for infection.
Obesity (high body weight) is linked to insulin resistance, often being cited as the cause, but more recently being proposed as a possible result of insulin resistance. The relationship is complex, and measures to control weight and reduce insulin resistance are important pieces in optimizing your terrain.66Diabesity: How Obesity Is Related to Diabetes. Cleveland Clinic. November 8, 2021. Viewed September 15, 2022.
Another two-way link is between hyperglycemia/insulin resistance and hormone imbalances. Diabetes itself is a hormone imbalance condition,67Are Diabetes and Hormonal Imbalances Linked? Matthews Internal Medicine. Viewed September 15, 2022. but other hormones besides insulin can be involved. For instance, low testosterone is common in men with diabetes and is linked to insulin resistance. Estrogen may increase insulin sensitivity, while progesterone may reduce that sensitivity.
When a person is under stress, the body increases its release of stress hormones (glucocorticoids) such as cortisol and epinephrine. These hormones can impair the effects of insulin and slow down glucose absorption,68Bauerle KT, Harris C. Glucocorticoids and diabetes. Missouri Medicine. 2016 Sep-Oct;113(5):378-383. ensuring enough glucose is in the blood to provide energy for the fight-or-flight response. If stress hormones remain high for a prolonged time, chronically high levels of glucose in the blood can develop.
Stress hormones surge during acute stress, but are also released in a daily up and down rhythm based on the body’s internal clock. For instance, stress hormones are normally lower during sleep and rise after waking. If these daily (circadian) rhythms are disrupted, such as from inadequate sleep or reversed sleep-wake times, hormones that affect glucose control, insulin resistance and basic metabolism can also get out of rhythm. In people with diabetes, these hormonal release rhythms may be disrupted, dangerously affecting blood sugar levels in the early morning.
Not only do stress hormones follow a daily rhythmic pattern, but other hormones as well, including hormones related to metabolism. “An intimate relationship between circadian clocks and endocrine systems exists. This relationship is clinically relevant since disruption of the circadian clock is linked to metabolic disease.”69Pillon NJ, Loos RJF, Marshall SM, Zierath JR. Metabolic consequences of obesity and type 2 diabetes: Balancing genes and environment for personalized care. Cell. 2021 Mar 18;184(6):1530-1544. Metabolic hormones such as leptin, insulin and others respond to fasting/feeding cycles. Eating late at night, when the body is normally expected to fast, is linked to overweight and poor glycemic control.
Your microbiomethe collection of microbes living on and within your body also influences and is influenced by glucose. Because of its important metabolic function, your microbiome may influence the development of both obesity and diabetes. An imbalanced gut microbiota is linked to impaired glycemic control and development of type 2 diabetes in the host.70Gérard C, Vidal H. Impact of gut microbiota on host glycemic control. Frontiers in Endocrinology (Lausanne). 2019 Jan 30;10:29.
Measures to improve the health of your microbiome, such as through a diet including foods that are fermented or high in fiber, may promote beneficial microorganisms and contribute to the health of your metabolism. Healthy fermented foods include yogurt, miso, tempeh, and fermented vegetables such as sauerkraut.
Bottom line: Insulin resistance and high blood glucose affect and/or are affected by all the other terrain factors. We recommend you work with your healthcare practitioner to determine which terrain imbalances you may have and what is driving those imbalances. Then you can make a plan to optimize your terrain in the most sensible way. For instance, if you have high blood sugar and insulin resistance as well as chronic sleep disruption, it may make sense not only to treat your blood sugar and insulin balance up front, but also to improve your sleep.
Find health professionals who specialize in managing body terrain ›
Connections to symptoms and side effects
Helpful links
References
