Laura Pole, RN, MSN, OCNS, Andy Jackson, ND, and Miki Scheidel reviewed and provided input on this post.
A substantial amount of evidence so far shows a lower risk of many types of cancerbreast cancer, colorectal cancer, gastrointestinal cancer, head and neck cancer, kidney cancer, lung cancer, lymphoma, melanoma, prostate cancer, and thyroid cancer among people with mid-range blood vitamin D levels compared to a deficiency (blood levels below 20 nanograms per milliliter, or ng/mL).1Hepp N, Ryan E. Vitamin D: How can vitamin D help me? What the research says. CancerChoices. September 4, 2022. Viewed September 7, 2022. Because roughly 40% of the adult populations of the US and Europe are deficient in vitamin D, and even higher levels of deficiency are seen among people with dark skin,2Cashman KD, Dowling KG et al. Vitamin D deficiency in Europe: pandemic? American Journal of Clinical Nutrition. 2016 Apr;103(4):1033-44; Parva NR, Tadepalli S et al. Prevalence of vitamin D deficiency and associated risk factors in the US population (2011-2012). Cureus. 2018 Jun 5;10(6):e2741; Forrest KY, Stuhldreher WL. Prevalence and correlates of vitamin D deficiency in US adults. Nutrition Research. 2011 Jan;31(1):48-54. the link between vitamin D deficiency and cancer risk deserves attention.
However, as we describe below, evidence also shows higher risk of some types of cancer among people with vitamin D blood levels above the middle range. Some studies suggest that men have lower optimal vitamin D levels than women. Understanding the optimal level for you and checking your blood vitamin D levels may be important in deciding whether to use vitamin D supplements. We have found evidence that supplements can be helpful in reducing cancer risk—but only among people with vitamin D deficiency.
We have found evidence that supplements can be helpful in reducing cancer risk—but only among people with vitamin D deficiency.
A recent report from New England Journal of Medicine › (NEJM) found no benefit on risk of bone fractures during five years of follow up among people taking vitamin D supplements. Some commentaries based on this study advocate that people stop taking vitamin D and even stop having vitamin D levels tested3Cummings SR, Rosen C. VITAL findings—a decisive verdict on vitamin D supplementation. New England Journal of Medicine. 2022 Jul 28;387(4):368-370.—advice we consider incomplete, since they are not accounting for the link between vitamin D levels and cancer risk.
The devil is in the details
We’ve done a broad and detailed review of the relationship between vitamin D and cancer. In all our reviews of complementary cancer therapies, we try to make sense of the available studies, sometimes numbering in the hundreds, by looking carefully at details such as comparison groups, doses, study populations, and timing (whether during cancer treatment or before diagnosis, for example).
We found a high level of variability across studies looking at vitamin D.
- Baseline tracking: Some studies of vitamin D supplements consider the starting (baseline) levels of vitamin D blood levels, usually reported as 25(OH)D levels, but others do not.
- Measurements: Some studies report 25(OH)D level as ng/mL, while others use nanomoles per liter (nmol/L), so the numbers don’t line up easily. (To interpret your own lab results, check which is used, and if needed, multiply nmol/L by 0.4 to convert to ng/mL).
- Deficiency levels: Some studies define “vitamin D deficiency” as 25(OH)D levels below 8 ng/mL, others define it as anything below 20 ng/mL, and yet other studies put it anywhere in between those levels or even leave it undefined.
- High blood levels: “High” blood levels of vitamin D reported in studies can be anywhere from 12 to 40 ng/mL or higher.
Where “low” and “high” levels fall on the researchers’ scale makes a big difference in interpreting study results. Without having a consistent starting line and measures, judging whether people are making progress toward their health goals by increasing vitamin D in their diets or taking supplements is challenging.
Vitamin D and cancer risk: more isn’t always better
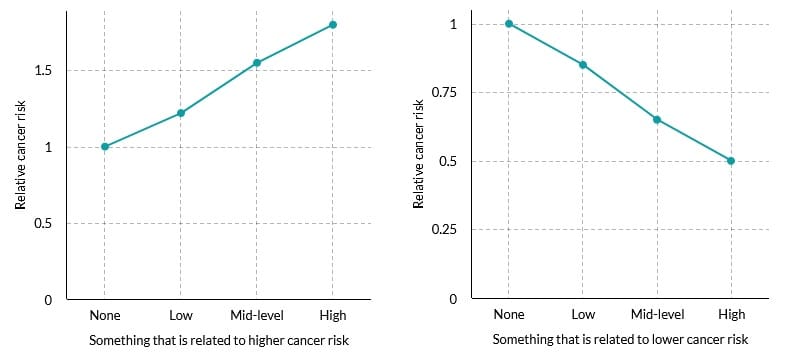
In many studies of vitamin D levels, researchers compare outcomes (cancer risk, for example) among people with the highest blood levels of vitamin D to the lowest levels. Comparing highest levels to lowest levels is a good approach when the relationship is linear—roughly in a straight line—as in the graphs in Figure 1 with made-up data showing higher risk of cancer with more of something on the left, and lower risk of cancer with more of something on the right. Researchers tend to like linear relationships—they’re easier to analyze and interpret than non-linear relationships with curvy lines. They even try to straighten out curvy lines, as we’ll see below.
But what if you have a nonlinear relationship—U-shaped or S-shaped—between vitamin D and cancer outcomes? With a U-shaped relationship, you’ll find higher risks of cancer with both low and high blood levels compared to mid-range levels. By comparing only the highest levels to the lowest levels and ignoring anything in between, you could find that there’s not much difference. That’s exactly what happened in a study of vitamin D and lung cancer, in which the researchers concluded “that the serum 25(OH)D level was not associated with the risk of lung cancer.” This was in a combined analysis of 12 studies, considered pretty good evidence.4Wei H, Jing H, Wei Q, Wei G, Heng Z. Associations of the risk of lung cancer with serum 25-hydroxyvitamin D level and dietary vitamin D intake: a dose-response PRISMA meta-analysis. Medicine (Baltimore). 2018 Sep;97(37):e12282.
But looking at the graph of the relationship from this article in Figure 2, you can see that the numbers at the low end and the high end of 25(OH)D levels do not tell the whole story.
In this graph, the solid curved line shows the risk of lung cancer as it relates to vitamin D blood levels. The dashed lines show the confidence intervals—a researcher’s way of saying that the results of any study, or even combined analysis of studies, contains error, but we have high confidence that most similar studies would get results in the zone between these 2 dashed lines. The dotted line is the attempt to make the very curvy solid line conform to a straight line so that we can interpret whether things are going up or down overall.
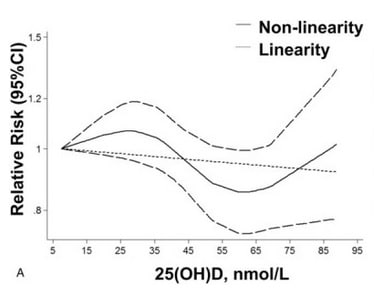
But the overall linear trend is not adequate to tell the story of a line that is as curvy as the solid line here. It looks as though the relative risk of lung cancer is higher than average (above 1) up to about 35 nmol/L of 25(OH)D, then drops quite a bit to be lower than average (below 1) until you get to somewhere around 70 nmol/L, at which point the risk starts rising, becoming higher than average (above 1 again) around 85 nmol/L. Comparing the relative risk of lung cancer among people with levels of 85-90 compared only to people with levels 5-35 would lead to the conclusion that vitamin D levels are not associated with risk of lung cancer—exactly what the researchers concluded. But what about that big dip in risk between about 45 and 70 nmol/L (about 18 and 28 ng/mL)? We don’t know if it’s meaningful or not because the researchers didn’t analyze it for significance.
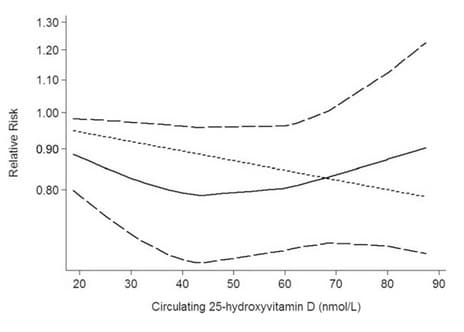
In Figure 3, we see a similar nonlinear pattern, a U-shaped relationship, in another combined analysis of lung cancer studies.6Feng Q, Zhang H, Dong Z, Zhou Y, Ma J. Circulating 25-hydroxyvitamin D and lung cancer risk and survival: a dose-response meta-analysis of prospective cohort studies. Medicine (Baltimore). 2017 Nov;96(45):e8613. Because the researchers analyzed only the dotted line (straightening out the U-shaped relationship from the solid line), they concluded that higher levels of vitamin D are linked to decreased risk of lung cancer. Analyses such as these may have contributed to some people’s thinking that more vitamin D is always better. But when we look at the actual relationship shown in the curved solid line, we find that higher vitamin D levels start showing an apparently higher risk of lung cancer compared to the sweet spot between about 35 and 70 nmol/L (about 14 and 28 ng/mL). But, again, this wasn’t analyzed for significance.
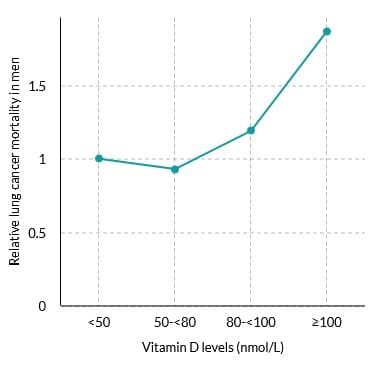
A separate, very large study looked at the risk of lung cancer mortality among men without cancer at the start and provided statistical analysis of the relationship with vitamin D levels. As shown in Figure 4, the study found 87% higher risk among men with 25(OH)D levels higher than 40 ng/mL (100 nmol/L) compared to levels lower than 20 ng/mL (50 nmol/L), although no link was found among women.8Freedman DM, Looker AC, Abnet CC, Linet MS, Graubard BI. Serum 25-hydroxyvitamin D and cancer mortality in the NHANES III study (1988-2006). Cancer Research. 2010 Nov 1;70(21):8587-97. This provides some evidence that the U-shaped curves in the graphs above may be meaningful. We’re left wondering what the line below 50 nmol/L looks like, however.
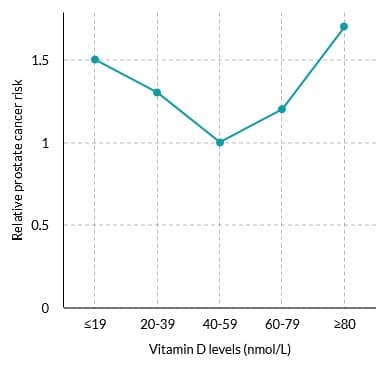
A U-shaped trend is also seen in studies of prostate cancer risk, with increases in cancer risk at both low10Kristal AR, Till C et al. Plasma vitamin D and prostate cancer risk: results from the Selenium and Vitamin E Cancer Prevention Trial. Cancer Epidemiology, Biomarkers and Prevention. 2014 Aug;23(8):1494-504; Tuohimaa P, Lyakhovich A et al. Vitamin D and prostate cancer. Journal of Steroid Biochemistry and Molecular Biology. 2001 Jan-Mar;76(1-5):125-34. and high11Xu Y, Shao X et al. Positive association between circulating 25-hydroxyvitamin D levels and prostate cancer risk: new findings from an updated meta-analysis. Journal of Cancer Research and Clinical Oncology. 2014 Sep;140(9):1465-77; Tuohimaa P, Tenkanen L et al. Both high and low levels of blood vitamin D are associated with a higher prostate cancer risk: a longitudinal, nested case-control study in the Nordic countries. International Journal of Cancer. 2004 Jan 1;108(1):104-8. levels of 25(OH)D compared to mid-range levels. As shown in Figure 5 from one large study, compared to people in the mid range (16-24 ng/mL, 40-59 nmol/L), people with high vitamin D levels (32 or more ng/mL, 80 or more nmol/L) had higher risk of prostate cancer, and people with levels either below 16 ng/mL (40 nmol/L) or between 24 and 32 ng/mL (60 and 79 nmol/L) showed trends toward higher risks.12Tuohimaa P, Tenkanen L et al. Both high and low levels of blood vitamin D are associated with a higher prostate cancer risk: a longitudinal, nested case-control study in the Nordic countries. International Journal of Cancer. 2004 Jan 1;108(1):104-8.
Not all cancer types show U-shaped curves, at least not in the ranges that have been studied. Our review of vitamin D › shows modest to good evidence of lower risk of many types of cancerbreast cancer, colorectal cancer, gastrointestinal cancer, head and neck cancer, kidney cancer, lung cancer, lymphoma, melanoma, prostate cancer, and thyroid cancer among people with higher vitamin D levels compared to people deficient in vitamin D. We don’t yet know the upper limit of benefit for many cancer types, but we see an upper limit for men regarding lung cancer and prostate cancer, and we have some indications of similar limits with pancreatic cancer and skin cancer. Higher vitamin D levels are not always better in terms of reducing cancer risk.
Higher vitamin D levels are not always better in terms of reducing cancer risk.
Bottom line: hit the sweet spot
Evidence so far shows a lower risk of many types of cancerbreast cancer, colorectal cancer, gastrointestinal cancer, head and neck cancer, kidney cancer, lung cancer, lymphoma, melanoma, prostate cancer, and thyroid cancer among people with mid-range blood vitamin D levels compared to lower levels. Scientific consensus puts the low end of the middle range at 20 ng/mL for everyone. Defining the upper limit exactly is extremely difficult because different studies report results in so many different ways, but so far it seems to be about 35 ng/mL for men. It may be higher than that for women. If you have 25(OH)D levels below 20 ng/mL, supplements that bring you up into the middle range might be beneficial.
However, if your blood level is in the middle range, taking vitamin D supplements might not bring much benefit regarding cancer risk. For men with vitamin D levels above the middle range, more vitamin D could be raising your risk of cancer as a whole and some types of cancer—lung cancer, pancreatic cancer, and prostate cancer—compared to the mid-range levels. This is why we’re concerned about advice not to have vitamin D blood levels tested—both low and high levels may need your attention. We don’t yet have enough information about cancer risk among women to know if high blood levels of vitamin D are linked to higher risk of cancer or how high those levels would be.
Getting your vitamin D levels to the appropriate range is only one of many steps you can take to improve your entire body terrainthe internal conditions of your body, including nutritional status, fitness, blood sugar balance, hormone balance, inflammation and more. You can find more about your body terrain and how to manage it in our handbook.
Learn more
References
Ms. Hepp is a researcher and communicator who has been writing and editing educational content on varied health topics for more than 20 years. She serves as lead researcher and writer for CancerChoices and also served as the first program manager. Her graduate work in research and cognitive psychology, her master’s degree in instructional design, and her certificate in web design have all guided her in writing and presenting information for a wide variety of audiences and uses. Nancy’s service as faculty development coordinator in the Department of Family Medicine at Wright State University also provided experience in medical research, plus insights into medical education and medical care from the professional’s perspective.
